Soap Format Medical Records - Each letter refers to one of four sections in the document. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently.
Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Each letter refers to one of four sections in the document. In the soap format, soap stands for subjective, objective, assessment, and plan.
Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. In the soap format, soap stands for subjective, objective, assessment, and plan. Each letter refers to one of four sections in the document.
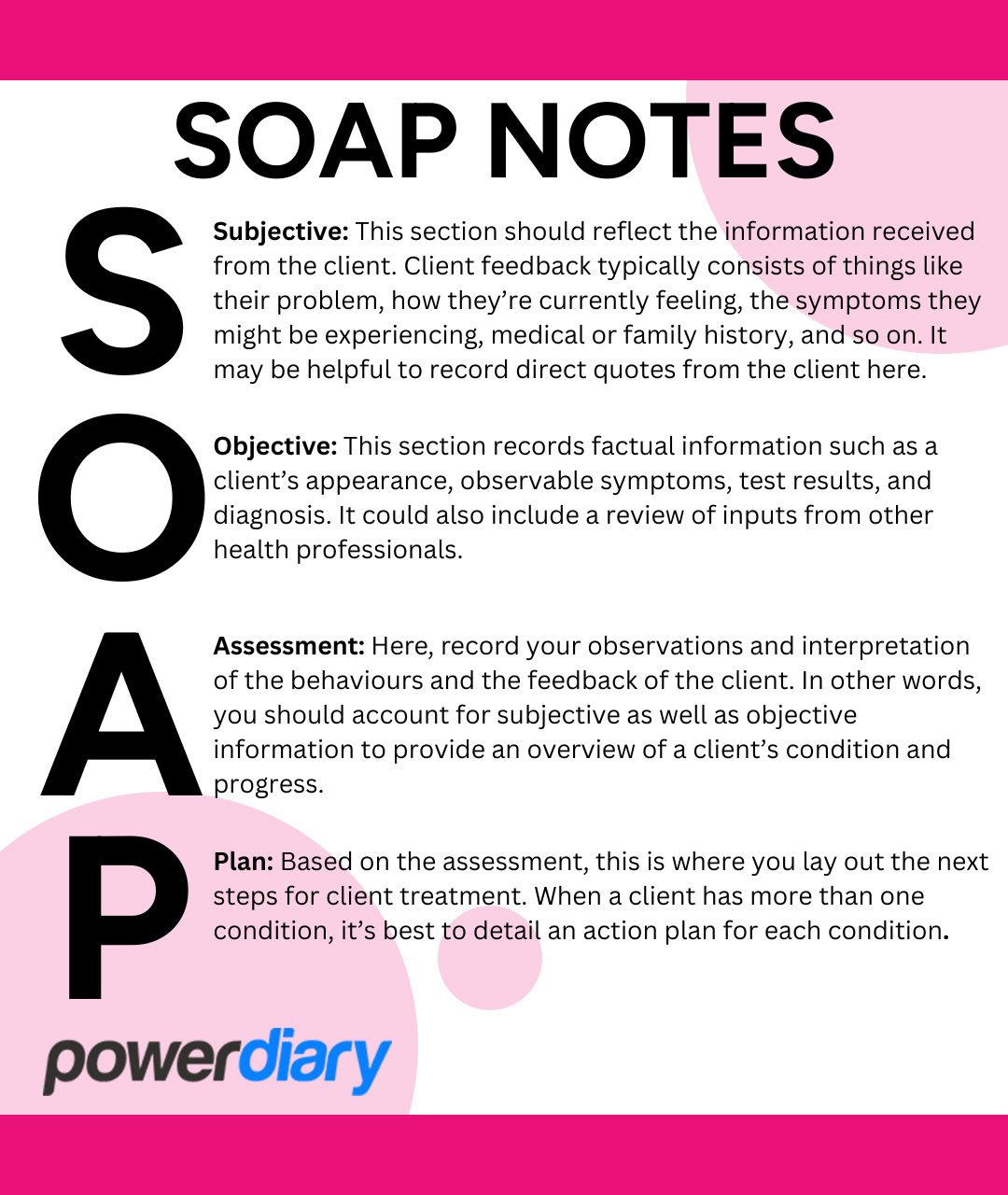
What’s the Difference SOAP Notes vs DAP Notes Power Diary
Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Each letter refers to one of four sections in the document. In the soap format, soap stands for subjective, objective, assessment, and plan.
How to Write Effective Massage Therapy SOAP Notes
Each letter refers to one of four sections in the document. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently.
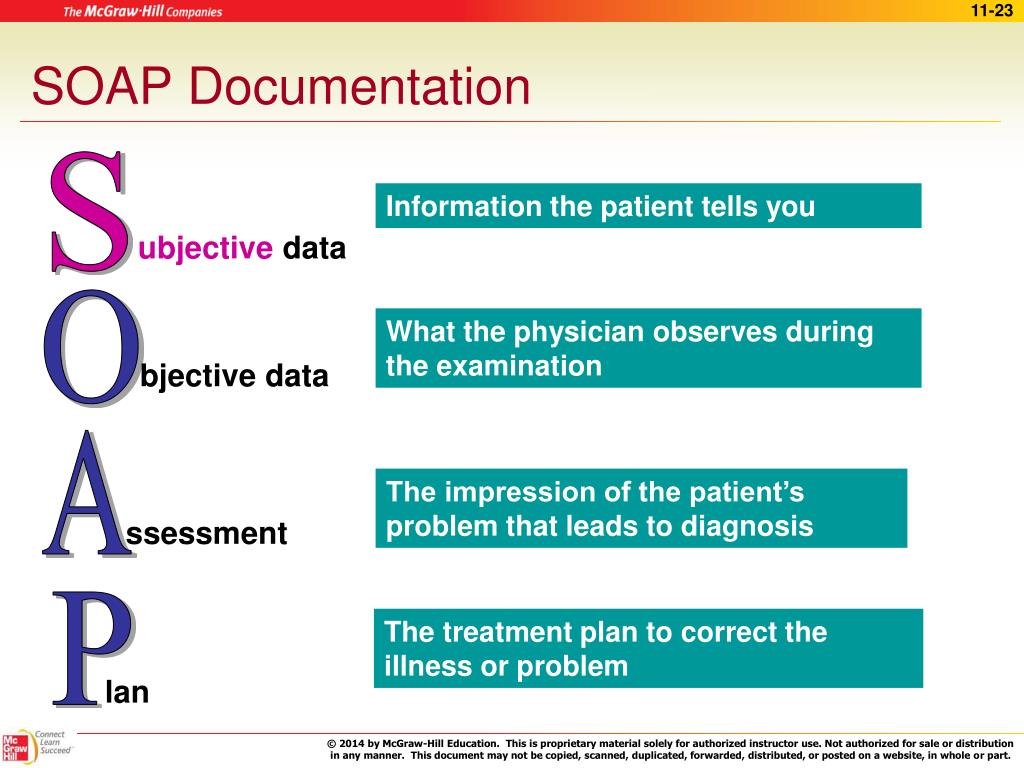
PPT Medical Records and Documentation PowerPoint Presentation, free
Each letter refers to one of four sections in the document. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently.
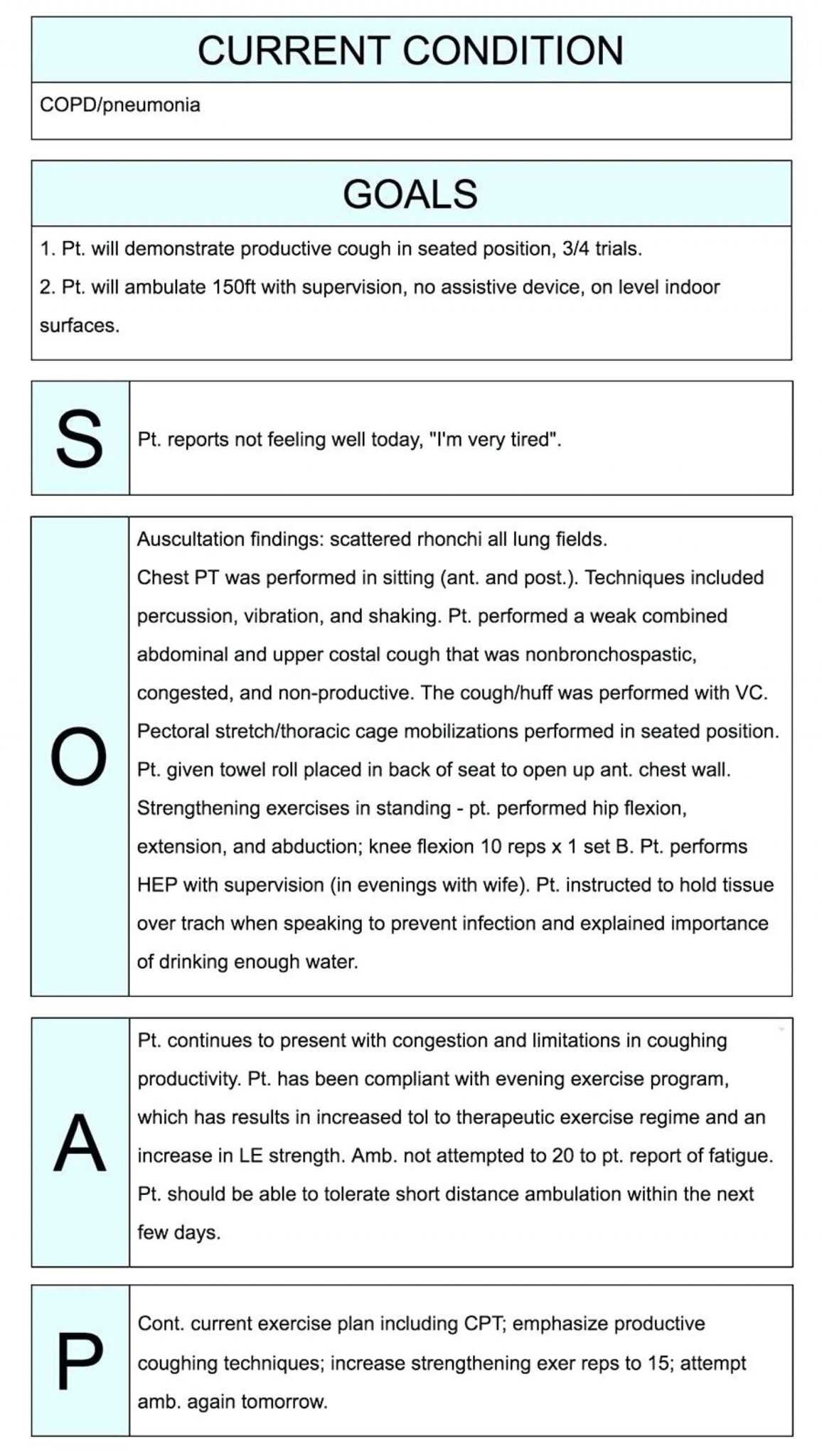
Documenting with SOAP Notes (2 CEs) Premier Continuing Education
In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Each letter refers to one of four sections in the document.
Occupational Therapy Documentation Tips The OT Toolbox Occupational
Each letter refers to one of four sections in the document. In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently.
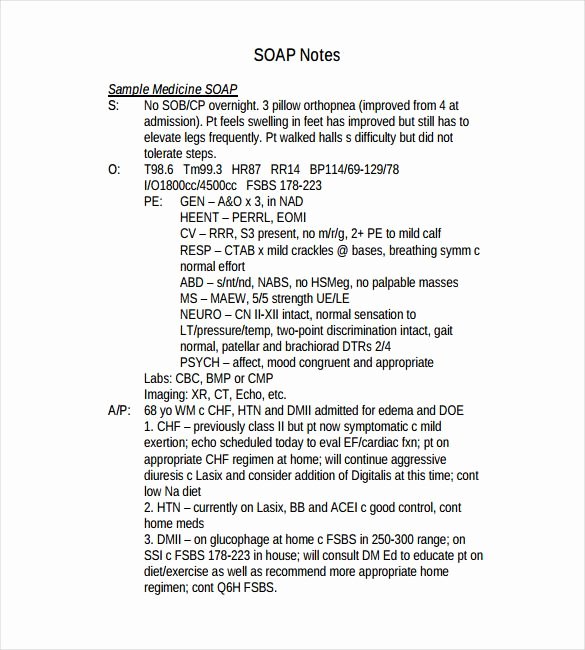
35 soap Charting Examples Hamiltonplastering
In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Each letter refers to one of four sections in the document.
Veterinary SOAP notes format of Electronic Health Records (EMRs) 2024
In the soap format, soap stands for subjective, objective, assessment, and plan. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Each letter refers to one of four sections in the document.
023 Soap Note Example Mental Health Ems Format Template inside Soap
Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. Each letter refers to one of four sections in the document. In the soap format, soap stands for subjective, objective, assessment, and plan.
Soap Format In Medical Records Soap Ideas
Each letter refers to one of four sections in the document. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently. In the soap format, soap stands for subjective, objective, assessment, and plan.
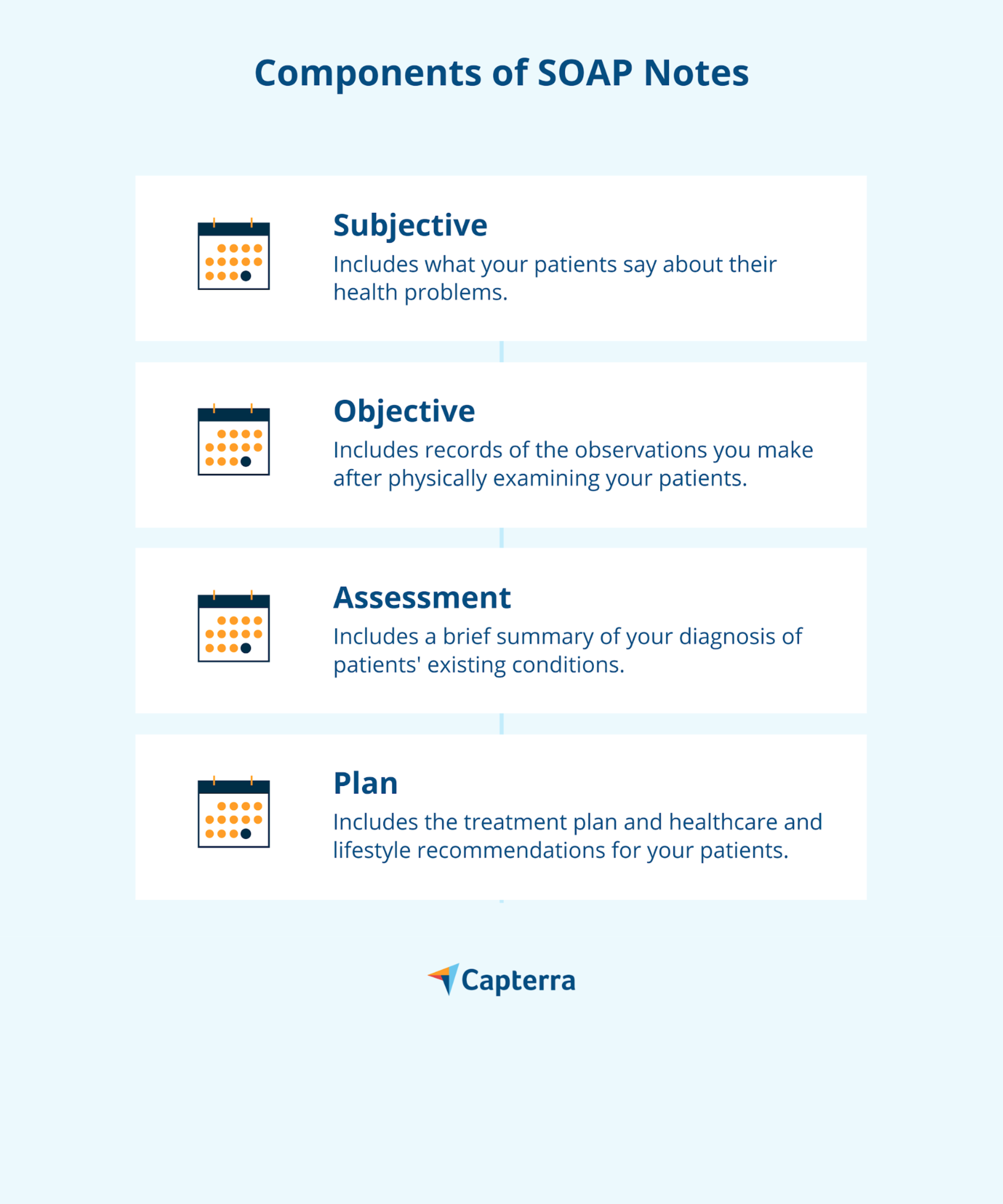
Free SOAP Notes Templates for Busy Healthcare Professionals Capterra
In the soap format, soap stands for subjective, objective, assessment, and plan. Each letter refers to one of four sections in the document. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently.
In The Soap Format, Soap Stands For Subjective, Objective, Assessment, And Plan.
Each letter refers to one of four sections in the document. Soap notes are a way for healthcare providers to document patient data more efficiently and consistently.