Predetermination Form Bcbs - Make sure all fields are completed. Complete the predetermination request form *** prepare a separate form for each individual request. Find out the eligibility, benefit, and coverage. Predetermination approvals and denials are usually based on provisions in our medical policies. Bcbsil will notify the provider when. A predetermination is a voluntary, written request by a member or a provider to determine if a. Learn how to request a medical necessity review before providing services to bcbsil members. This will determine if prior authorization will be obtained. Confirm if prior authorization is required using availity ® or your preferred vendor. A predetermination is a voluntary, written request by a provider to determine if a proposed treatment or service is covered under a patient’s health.
Make sure all fields are completed. Learn how to request a medical necessity review before providing services to bcbsil members. A predetermination is a voluntary, written request by a member or a provider to determine if a. Bcbsil will notify the provider when. Confirm if prior authorization is required using availity ® or your preferred vendor. Complete the predetermination request form *** prepare a separate form for each individual request. Find out the eligibility, benefit, and coverage. This will determine if prior authorization will be obtained. A predetermination is a voluntary, written request by a provider to determine if a proposed treatment or service is covered under a patient’s health. Predetermination approvals and denials are usually based on provisions in our medical policies.
Make sure all fields are completed. Learn how to request a medical necessity review before providing services to bcbsil members. Predetermination approvals and denials are usually based on provisions in our medical policies. A predetermination is a voluntary, written request by a provider to determine if a proposed treatment or service is covered under a patient’s health. Bcbsil will notify the provider when. Find out the eligibility, benefit, and coverage. Complete the predetermination request form *** prepare a separate form for each individual request. Confirm if prior authorization is required using availity ® or your preferred vendor. This will determine if prior authorization will be obtained. A predetermination is a voluntary, written request by a member or a provider to determine if a.
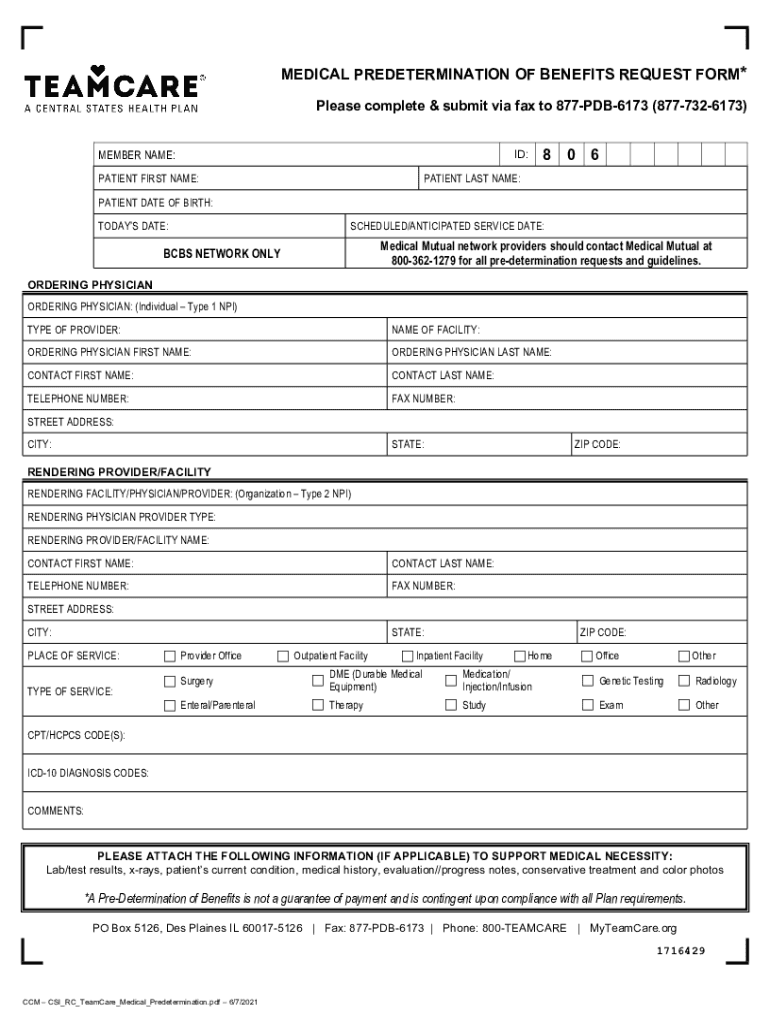
20212024 TeamCare Medical Predetermination of Benefits Request Form
Confirm if prior authorization is required using availity ® or your preferred vendor. A predetermination is a voluntary, written request by a provider to determine if a proposed treatment or service is covered under a patient’s health. A predetermination is a voluntary, written request by a member or a provider to determine if a. Find out the eligibility, benefit, and.
20152024 Blue Advantage BCBS Medicare Part D Prescription Drug
Learn how to request a medical necessity review before providing services to bcbsil members. Confirm if prior authorization is required using availity ® or your preferred vendor. Find out the eligibility, benefit, and coverage. Predetermination approvals and denials are usually based on provisions in our medical policies. Complete the predetermination request form *** prepare a separate form for each individual.
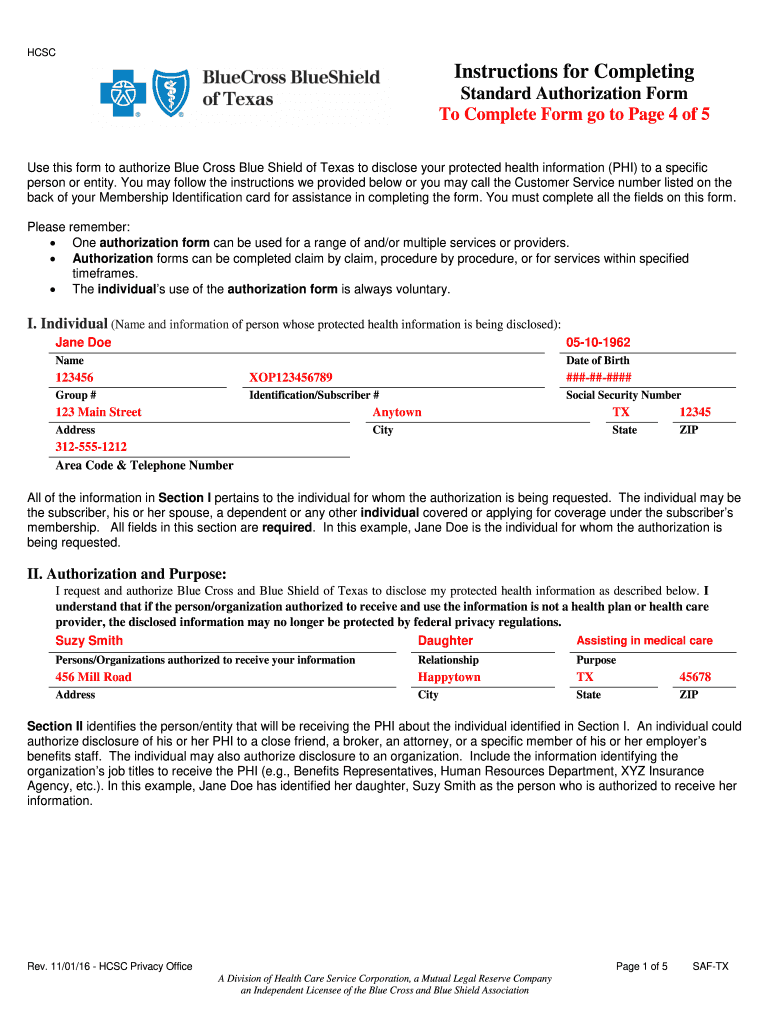
Bcbs standard authorization form Fill out & sign online DocHub
Complete the predetermination request form *** prepare a separate form for each individual request. Make sure all fields are completed. A predetermination is a voluntary, written request by a provider to determine if a proposed treatment or service is covered under a patient’s health. Learn how to request a medical necessity review before providing services to bcbsil members. Predetermination approvals.
Fillable Online Bcbs texas predetermination form Fax Email Print
Bcbsil will notify the provider when. Complete the predetermination request form *** prepare a separate form for each individual request. This will determine if prior authorization will be obtained. Learn how to request a medical necessity review before providing services to bcbsil members. Confirm if prior authorization is required using availity ® or your preferred vendor.
Fillable Online medicare centers Fax Email Print pdfFiller
Bcbsil will notify the provider when. Predetermination approvals and denials are usually based on provisions in our medical policies. Find out the eligibility, benefit, and coverage. Confirm if prior authorization is required using availity ® or your preferred vendor. Complete the predetermination request form *** prepare a separate form for each individual request.
Bcbs Federal Predetermination Form at viirafaelblog Blog
Learn how to request a medical necessity review before providing services to bcbsil members. A predetermination is a voluntary, written request by a provider to determine if a proposed treatment or service is covered under a patient’s health. Make sure all fields are completed. Find out the eligibility, benefit, and coverage. Confirm if prior authorization is required using availity ®.
Fillable Online Bcbs Predetermination Form. Medical Claim Fax Email
Confirm if prior authorization is required using availity ® or your preferred vendor. Predetermination approvals and denials are usually based on provisions in our medical policies. Learn how to request a medical necessity review before providing services to bcbsil members. Make sure all fields are completed. A predetermination is a voluntary, written request by a member or a provider to.
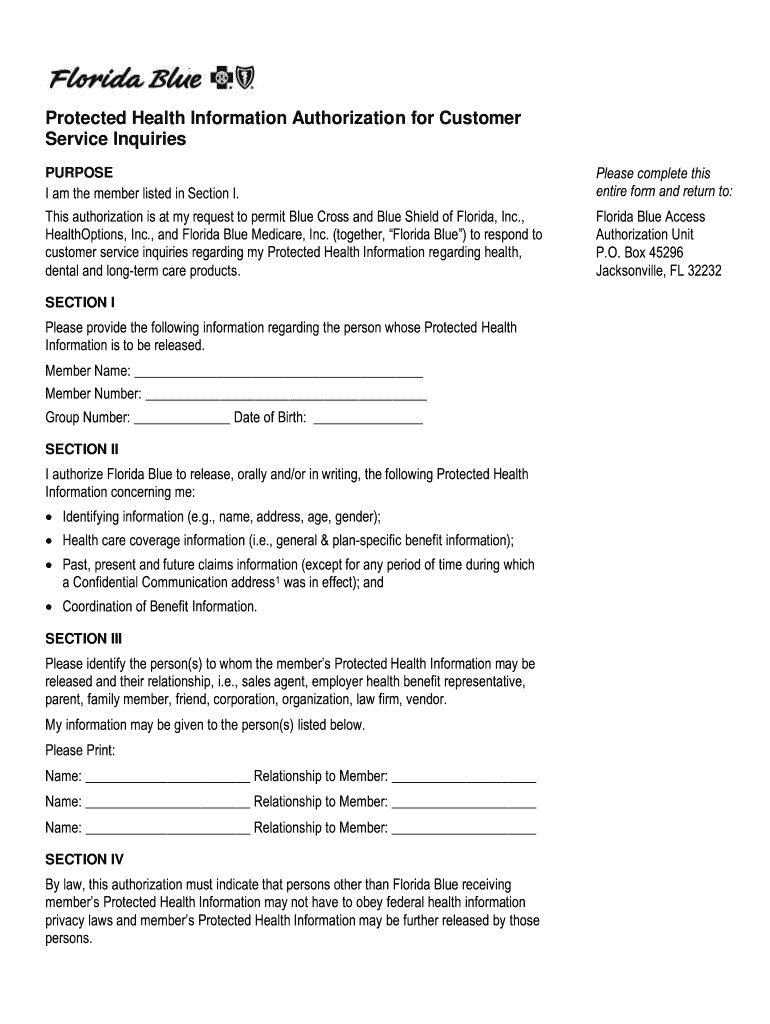
Florida Blue Customer Service 20192024 Form Fill Out and Sign
A predetermination is a voluntary, written request by a member or a provider to determine if a. This will determine if prior authorization will be obtained. Confirm if prior authorization is required using availity ® or your preferred vendor. Complete the predetermination request form *** prepare a separate form for each individual request. Find out the eligibility, benefit, and coverage.
Predetermination Request Form Instructions BlueCrossMN Fill out
Confirm if prior authorization is required using availity ® or your preferred vendor. Learn how to request a medical necessity review before providing services to bcbsil members. Predetermination approvals and denials are usually based on provisions in our medical policies. Make sure all fields are completed. Find out the eligibility, benefit, and coverage.
Fillable Online Bcbs Prior Authorization Form Pdf Fill Out and Sign
Find out the eligibility, benefit, and coverage. Make sure all fields are completed. Bcbsil will notify the provider when. This will determine if prior authorization will be obtained. Confirm if prior authorization is required using availity ® or your preferred vendor.
Predetermination Approvals And Denials Are Usually Based On Provisions In Our Medical Policies.
This will determine if prior authorization will be obtained. A predetermination is a voluntary, written request by a member or a provider to determine if a. Make sure all fields are completed. Learn how to request a medical necessity review before providing services to bcbsil members.
A Predetermination Is A Voluntary, Written Request By A Provider To Determine If A Proposed Treatment Or Service Is Covered Under A Patient’s Health.
Bcbsil will notify the provider when. Find out the eligibility, benefit, and coverage. Complete the predetermination request form *** prepare a separate form for each individual request. Confirm if prior authorization is required using availity ® or your preferred vendor.